The treatment of triple negative breast cancer (TNBC) has always involved surgery. This can be in the form of a lumpectomy (preserving the breast) or of a mastectomy (removing the breast). However, the disease can often be eradicated prior to surgery due to advances in chemotherapy and immunotherapy. A clinical trial is now evaluating whether surgery can be avoided after chemotherapy. We would like to inform you of this trial.
TNBC and Neo-adjuvant Chemotherapy.
Sometimes chemotherapy and/or immunotherapy is administered to selected TNBC patients before surgery. The diagnosis of triple negative breast cancer is established with a core needle biopsy of the breast cancer. Sometimes the lymph nodes are also biopsied if they are abnormal. The patient will then receive chemotherapy +/- immunotherapy. At the end of treatment, they are re-evaluated again to decide what type of operation they need. Surgery is then performed, but in approximately 30 to 50% of women no cancer is found after the tissues are analyzed! This is what we call a pathologic complete response (PCR).
Surgeons started to wonder, “Is there a group of patients that doesn’t need surgery?” In 2014, researchers from the MD Anderson Cancer Center, The Mayo Clinic, Duke University, Pittsburgh Medical Center, Columbia University, The Carolinas Medical Center and The University of Texas Southwestern Medical Center reported their results. They included 170 triple negative breast cancer patients treated with chemotherapy prior to surgery. In 34.5% of those patients there was no cancer at the time of operation. They had achieved a, “Pathologic Complete Response (PCR)”. Even though there was no way to know of it before surgery, 34.5% of patients did not have cancer after chemotherapy.
Exciting New Findings!
Doctors at the MD Anderson Cancer Center in Houston then conducted another study. Forty patients were evaluated before and after chemotherapy. A minimally invasive vacuum assisted core biopsy of the tumor site was performed after the conclusion of chemotherapy. Finally, surgical removal of the initial cancer site was performed.
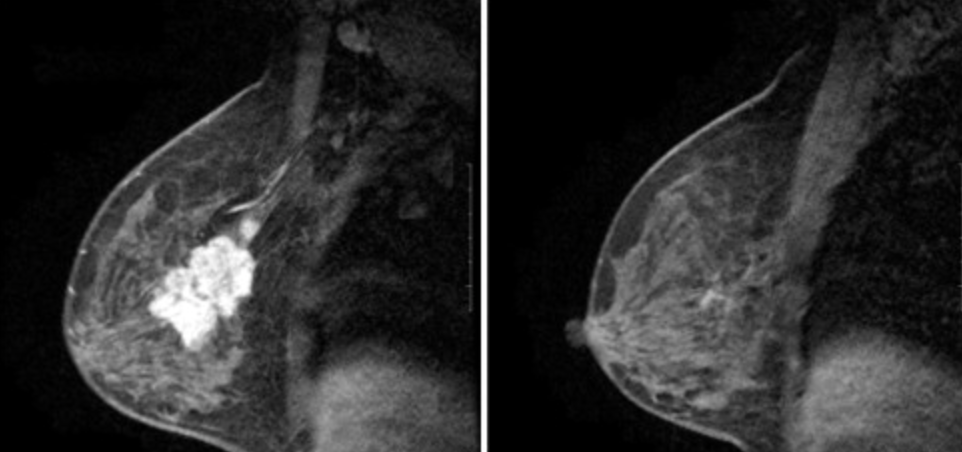
Close to half of the patients achieved a pathologic complete response (PCR) in the breast. What was very striking in that group of patients was that even those who initially had cancer in their axillary nodes were also able to clear their lymph nodes! In fact, the nodes were also clear in 97.5% of patients who had a pathologic complete response in the breast. This would indicate that if chemotherapy is able to eradicate the cancer in the breast, it can also eradicate it in the lymph nodes. So, follow my train of thought here. If we can give chemotherapy and eradicate the cancer in the breast and lymph nodes, then maybe all we need to do is re-biopsy the breast with a minimally invasive biopsy. That patient might not need surgery if there’s no cancer found in the biopsy!
Can We Avoid Surgery?
A large collaborative trial is underway. The MD Anderson Cancer Center together with partners from their network is spearheading a multicenter trial. It also involves the Mayo Clinic, The Carolinas Medical Center, and the University of Pittsburgh. They are enrolling patients with breast cancer who will complete neo-adjuvant chemotherapy. Many of these will be triple negative breast cancer patients. At the end of chemotherapy, they will undergo image-guided, vacuum-assisted biopsies of the primary breast tumor site. Patients who don’t have any residual cancer on biopsy will receive radiation therapy without surgery. Patients who do have residual cancer will receive standard surgery and radiation. The patients in this study will be evaluated every six months. The primary end-point of the study is to determine the rate of recurrence in the breast or axillary lymph nodes for both groups.
How do I get in a study? I just had a peanut piece size tumor removed that came back as triple negative metoplastic sarcoidanoma carcinoma. Margins were clean and benign I’m looking for options.
Clinicaltrials.gov will provide you with a comprehensive list of clinical trials. However, for an early stage TNBC as you describe, standard therapy has been shown to be very successful. Dr. Diehl