New nerve blocks called PECS Blocks are improving the quality of life of patients needing surgery to treat their breast cancer. Major breast surgery such as mastectomy with or without reconstruction is often associated with moderate to severe pain. Intravenous and oral pain killers such as Opioids are traditionally prescribed during and after surgery to relieve the pain. Opioids are associated with multiple side effects including nausea, vomiting, sedation, dizziness, constipation, tolerance, and dependence. Breast surgery itself frequently results in nausea and pain.
Reducing Side Effects From Surgery with PECS Blocks
Highly specialized nerve blocks can now reduce the side effects and pain that result from breast cancer surgery. PECS 1 and 2 blocks are what we call interfacial plane blocks – the injection of long acting local anesthetics into the potential space between the muscles in close proximity to the breast. Thus, injecting the long acting anesthetics between the pectoralis major and pectoralis minor muscles (PECS 1) and between the pectoralis minor and serratus anterior muscles (PECS 2) provides a high degree of pain relief during and after surgery. The nerves that go to the breast are located in the spaces between the muscles and numbed by the local anesthetics.
Strong Scientific Evidence
Multiple meta-analyses of randomized controlled studies have proven its benefit since this technique was first described in 2012 (1,2,3,4,5,6). Thus PECS blocks have become the foundation of a multi-pronged approach to pain control following breast surgery. Other medications including acetaminophen (Tylenol), nonsteroidal anti-inflammatory medications (Toradol), and GABA analogues (Gabapentin) , reduce or eliminate postoperative opioid requirements. This dramatic reduction in pain results in a much improved experience for the patient. Liposome encapsulated bupivacaine (Exparel) is a new long acting local anesthetic that can be added for even longer lasting relief. PECS 1 and PECS 2 blocks are performed by the anesthesiologist with ultrasound guidance under sedation prior to surgery or in the operating room after the patient is asleep. See figures 1 and 2.
After surgery, patients often describe a feeling of tightness at the mastectomy site but minimal sharp pain. When the surgery is carried down lower on the chest wall it can extend beyond the area covered by the block. In this case, the surgeon can supplement the block with additional local anesthetic injected along the inferior margin during surgery. Recent literature has described additional blocks that also provide pain relief after mastectomy.
Mastectomies As An Outpatient Procedure
In today’s environment of opioid dependance and Covid-19 pandemics, PECS blocks not only reduce the patient’s pain and need for exposure to opioids but can also reduce length of hospital stay for post-operative pain management. This has resulted in a trend towards outpatient surgery. Most mastectomies prior to the COVID-19 pandemic were performed in the hospital with an overnight stay. But during the pandemic this was not possible yet patients still required surgery. We and other institutions found that the routine use of PECS blocks and a multi-modal pain management regimen allowed us to move this surgery from the in-patient hospital setting to an out-patient same day surgery setting. This improved the patient experience and made it a safer operation.

Figure 1. Placement of needle with ultrasound guidance with the patient sedated or under anesthesia.
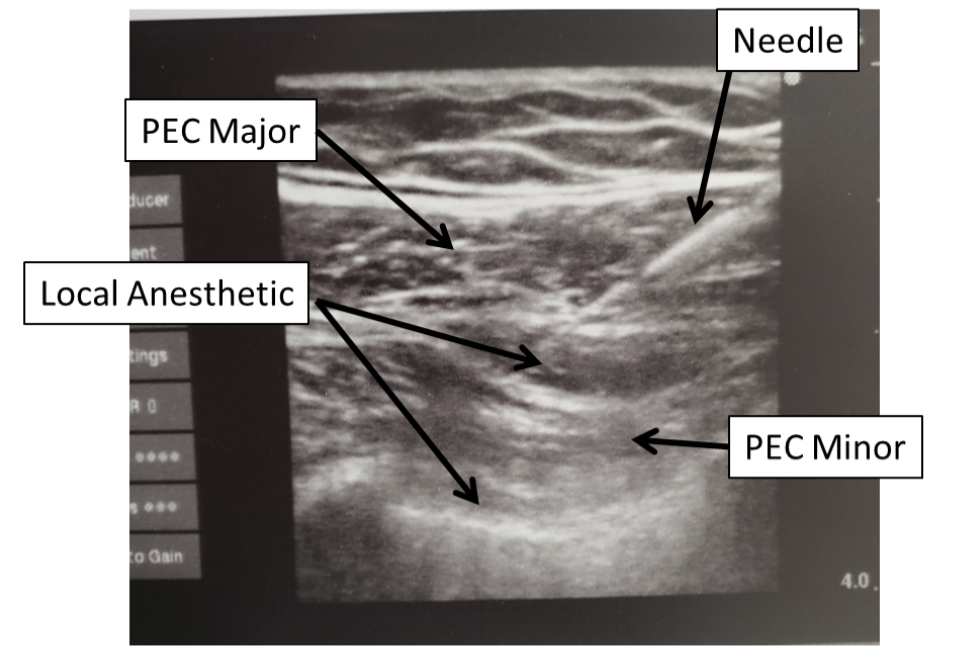
Figure 2. Ultrasound image of injection showing placement of local anesthetic between layers of muscle.
References:
1.Medicine (Baltimore). 2020 Apr;99(14):e19614. doi: 10.1097/MD.0000000000019614.
Clinical analgesic efficacy of pectoral nerve block in patients undergoing breast cancer surgery: A systematic review and meta-analysis.Sun Q(1), Liu S(1), Wu H(2), Kang W(3), Dong S(1), Cui Y(1), Pan Z(1), Liu K(4).
2.Int J Physiol Pathophysiol Pharmacol. 2020 Feb 25;12(1):40-50. eCollection 2020.
Pectoral Nerve (PECs) block for postoperative analgesia-a systematic review and meta-analysis with trial sequential analysis.Jin Z(1), Li R(1), Gan TJ(1), He Y(2), Lin J(1)
3.J Clin Anesth. 2020 Aug;63:109744. doi: 10.1016/j.jclinane.2020.109744. Epub 2020 Feb 25.
Analgesic efficacy of PECS and serratus plane blocks after breast surgery: A systematic review, meta-analysis and trial sequential analysis.Grape S(1), Jaunin E(1), El-Boghdadly K(2), Chan V(3), Albrecht E(4).
4.Reg Anesth Pain Med. 2019 Aug 9:rapm-2019-100658. doi: 10.1136/rapm-2019-100658. Online ahead of print.
Pectoral nerve blocks and postoperative pain outcomes after mastectomy: a meta-analysis of randomized controlled trials. Lovett-Carter D(1), Kendall MC(1), McCormick ZL(2), Suh EI(1), Cohen AD(1), De Oliveira GS(3).
5.Medicine (Baltimore). 2019 May;98(18):e15423. doi: 10.1097/MD.0000000000015423.
Pectoral nerve block in anesthesia for modified radical mastectomy: A meta-analysis based on randomized controlled trials.Zhao J(1), Han F(1), Yang Y(1), Li H(2), Li Z(1).
6.Anaesthesia. 2019 May;74(5):663-673. doi: 10.1111/anae.14607.
Analgesic efficacy of the Pecs II block: a systematic review and meta-analysis. Versyck B(1), van Geffen GJ(2), Chin KJ(3).